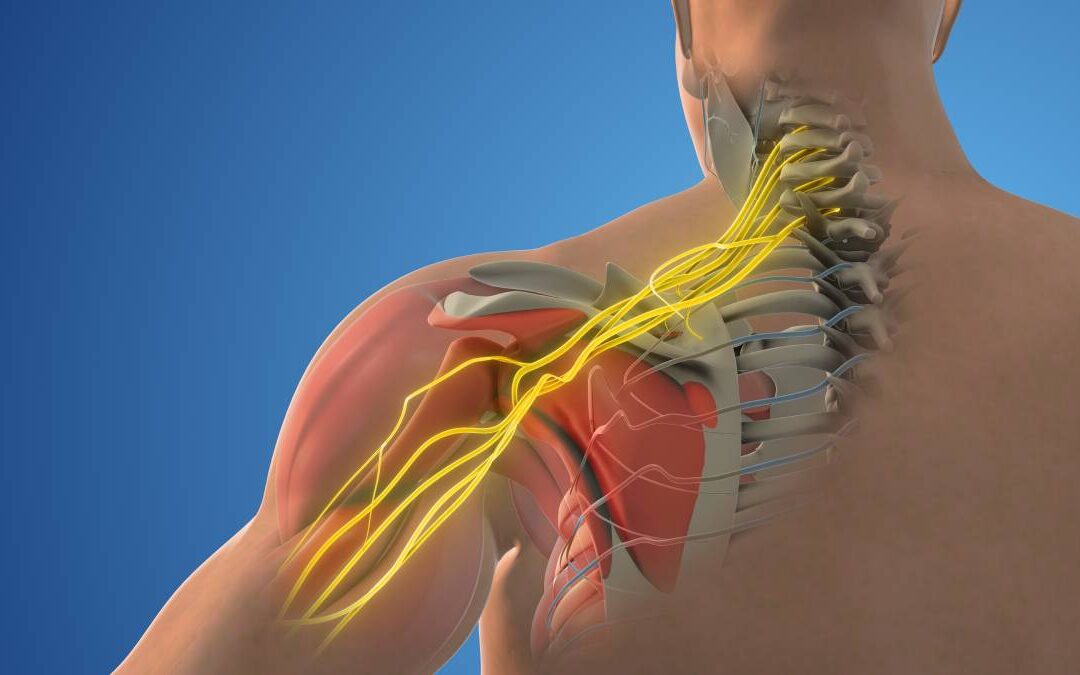
Nerve blocks are commonly used in anesthesia to provide targeted pain relief by interrupting nerve signal transmission. Despite their widespread use and general safety, neurological complications can occur, albeit rarely. Understanding the neurological complications of nerve blocks is essential for clinicians to effectively manage and mitigate risk.
Neurological complications of nerve blocks can range from transient symptoms to permanent deficits. The most frequently encountered problems include paresthesias, persistent pain, and motor weakness. These symptoms can result from direct nerve trauma, intraneural injection, or ischemic injury. Paresthesia, characterized by abnormal sensations such as tingling or burning, is often the first sign of nerve injury. While many cases resolve spontaneously within a few days, persistent symptoms warrant further investigation (1).
Direct nerve trauma is a major cause of neurological complications. It can occur when the needle or catheter injures the nerve during placement. In severe cases, this can lead to neuroma formation characterized by disorganized nerve growth and chronic pain. Proper technique and the use of ultrasound guidance have been shown to reduce the incidence of these injuries, highlighting the importance of skill and technology in preventing complications (2).
Intraneural injection, where the anesthetic is inadvertently injected into the nerve, can cause significant damage. This complication is of particular concern because it can result in high local concentrations of anesthetic, leading to neurotoxicity. Clinical studies have shown that intraneural injections can cause severe and prolonged neurological deficits, including motor weakness and sensory loss. The use of low-pressure injection techniques and real-time imaging can help minimize this risk (3).
Although less common, ischemic injury can also lead to neurological complications. It occurs when the blood supply to the nerve is compromised, either by direct compression from the injected volume or by vasoconstriction caused by the anesthetic itself. This can lead to nerve ischemia and subsequent damage that manifests as delayed-onset neuropathy. Research suggests that the choice of anesthetic and its concentration may influence the likelihood of ischemic injury, with lower concentrations being safer for peripheral nerves (4).
Patient-related factors also play a role in the risk of neurological complications following nerve blocks. Conditions such as diabetes, peripheral vascular disease, and pre-existing neuropathy can increase susceptibility to nerve injury. These factors highlight the need for a thorough preprocedural assessment to identify high-risk patients and tailor the anesthetic approach accordingly (5).
Despite these risks, the benefits of nerve blocks for effective pain management are well documented. The majority of neurological complications are transient and resolve without long-term sequelae. However, the potential for permanent deficits requires a cautious and informed approach to their use. Clinicians must weigh the benefits of nerve blocks against the risks and employ strategies to minimize complications, such as the use of advanced imaging techniques and adherence to recommended injection pressures.
In conclusion, while nerve blocks are a valuable tool in pain management, they carry a risk of neurological complications. These complications can result from direct nerve trauma, intraneural injection, and ischemic injury, with patient-related factors also influencing outcomes. Ongoing research and adherence to best practices are essential to reduce the incidence of these complications and ensure patient safety.
References
- Neal JM, Barrington MJ, Brull R, et al. The Second ASRA Practice Advisory on Neurologic Complications Associated With Regional Anesthesia and Pain Medicine: Executive Summary 2015. Reg Anesth Pain Med. 2015;40(5):401-430. doi:10.1097/AAP.0000000000000286
- Liu SS, Ngeow JE, Yadeau JT. Ultrasound-guided regional anesthesia and analgesia: a qualitative systematic review. Reg Anesth Pain Med. 2009;34(1):47-59. doi:10.1097/AAP.0b013e3181933ec3
- Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104(4):965-974. doi:10.1213/01.ane.0000258740.17193.ec
- Rice AS, McMahon SB. Peripheral nerve injury caused by injection needles used in regioUnderstanding the neurological complications of nerve blocks is essential for clinicians to effectively manage and mitigate risk.nal anaesthesia: influence of bevel configuration, studied in a rat model. Br J Anaesth. 1992;69(5):433-438. doi:10.1093/bja/69.5.433
- Jeng CL, Torrillo TM, Rosenblatt MA. Complications of peripheral nerve blocks. Br J Anaesth. 2010;105 Suppl 1:i97-i107. doi:10.1093/bja/aeq273






Recent Comments