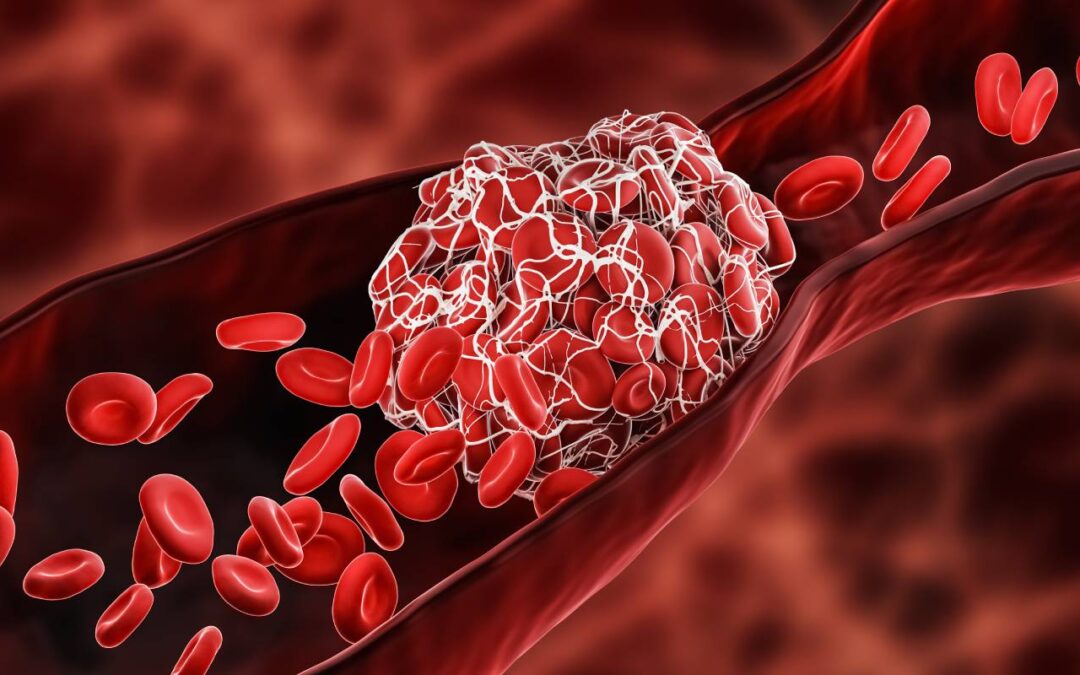
Having a sedentary lifestyle is associated with a number of serious non-communicable diseases, including heart disease, diabetes, osteoporosis, and colon cancer [1]. One of the most acutely perilous conditions that results from a sedentary lifestyle is a venous thromboembolism, which refers to when blood clots form – typically in the deep veins of the pelvis or the legs – and then become dislodged. Circulatory flow then deposits the clot elsewhere, thereby partially or completely obstructing blood flow. The severity of the venous thromboembolism depends heavily on the size of the clot and the area of deposition. For example, a deep venous thrombosis can be asymptomatic, but a clot which travels to the lungs and causes a pulmonary embolism is life-threatening [2].
Interestingly, case-control studies have shown that chronic exercise can decrease the risk of a venous thromboembolism by up to fifty percent [3]. While there is a clear correlation between lifestyle and blood clot risk, it remains somewhat unclear the exact mechanism behind the formation of blood clots due to a sedentary lifestyle. A number of factors are likely at play: for example, women with higher levels of physical activity/fitness were shown to have lower platelet activity than those who were less fit [4]. Platelet activation is the mechanism for blood clot formation, which may explain the reason that less fit individuals are more likely to experience a venous thromboembolism than more fit individuals. Another potential factor could be that muscular contraction “massages” the blood in the veins, causing minor clots to break down before they can accumulate more platelets and grow to a threatening size.
Somewhat paradoxically, exercise in the short term has been associated with both an increased and decreased risk of deep vein thrombosis [3]. Outcome appears to vary by patient demographic, particularly age and history of previous deep vein thrombosis, as well as overall frequency of exercise. Acute aerobic exercise, for example, appears to be correlated with greater blood clot risk, particularly for older patients who are not used to exercising.5 This can be explained in several ways. Firstly, acute aerobic exercise causes increased tissue stress, which can promote the formation of a blood clot or dislodge an existing blood clot [3,4,5]. This differs from chronic exercise, which conditions the body and makes instances of exercise less acutely stressful and can prevent clot formation in the first place. Therefore, the difference between whether exercise is helpful or harmful largely depends on approach. For individuals with a history of deep vein thrombosis, “weekend-warrior” type activities may exacerbate their condition, whereas those that have been doing casual aerobic workouts consistently are less likely to develop deep vein thrombosis in the first place.
Risk of a venous thromboembolism can be assessed using several different tests [6]. Levels of the plasma protein D-dimer, which is produced during blood clot dissolution, correlates with overall risk of deep vein thrombosis. Ultrasounds can be used to assess overall blood flow or monitor the progression of an existing clot. In extreme cases, a venography or MRI may be performed to assess overall circulation.
Following diagnosis of a blood clot, several therapies may be employed [4]. Typically, the first line of therapy involves taking an anticoagulant, which promotes blood clot dissolution. More severe cases may require a strong thrombolytic or a filter to prevent clots from causing a pulmonary embolism. Long-term solutions to reduce the risk of blood clots include a healthier, less sedentary lifestyle and the management of other comorbid conditions, such as cardiovascular disease or obesity.
References
1. World Health Organization. (2002). Physical inactivity a leading cause of disease and disability, warns who. World Health Organization. Retrieved from https://www.who.int/news/item/04-04-2002-physical-inactivity-a-leading-cause-of-disease-and-disability-warns-who
2. Essien, E. O., Rali, P., & Mathai, S. C. (2019). Pulmonary Embolism. The Medical clinics of North America, 103(3), 549–564. https://doi.org/10.1016/j.mcna.2018.12.013
3. Kabrhel, C., Varraso, R., Goldhaber, S. Z., Rimm, E., & Camargo, C. A., Jr (2011). Physical inactivity and idiopathic pulmonary embolism in women: prospective study. BMJ (Clinical research ed.), 343, d3867. https://doi.org/10.1136/bmj.d3867
4. Heber, S., Assinger, A., Pokan, R., & Volf, I. (2016). Correlation between Cardiorespiratory Fitness and Platelet Function in Healthy Women. Medicine and science in sports and exercise, 48(6), 1101–1110. https://doi.org/10.1249/MSS.0000000000000882
5. Bacon, S. L., Pelletier, R., & Lavoie, K. L. (2009). The impact of acute and chronic exercise on thrombosis in cardiovascular disease. Thrombosis and haemostasis, 101(3), 452–459.
6. Mayo Foundation for Medical Education and Research. (2020, December 22). Deep vein thrombosis (DVT). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/diagnosis-treatment/drc-20352563






Recent Comments