Neuromuscular blockades are typically performed during anesthesia in order to facilitate successful endotracheal intubation and provide optimal conditions for surgery by preventing patient movement. Monitoring neuromuscular blockade is a vital aspect of perioperative care, ensuring the precise administration and reversal of muscle relaxants, and assessing recovery. Inadequate monitoring of neuromuscular blockade can lead to complications, such as residual paralysis, delayed recovery, and respiratory compromise.
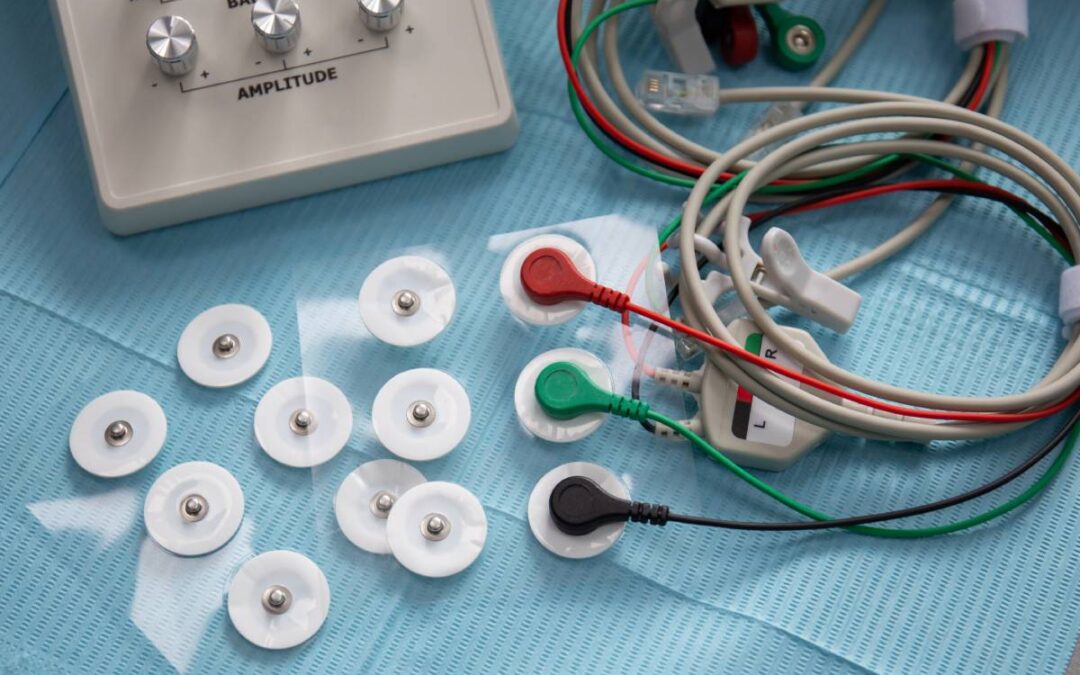
Monitoring neuromuscular blockade is best done with quantitative measures such as electromyography (EMG) or kinemyography to monitor both the administration and recovery from blocking agents [1]. Guidelines for monitoring state that if a quantitative monitor is not directly available, the use of a peripheral nerve stimulator is mandatory. This is due to the unreliable nature of a physical evaluation to determine potential weakness and residual paralysis from a neuromuscular blockade [2]. Several different nerves can be monitored, including the ulnar nerve, facial nerve, or posterior tibial nerve. The ulnar nerve has demonstrated higher accuracy than the facial nerve and thus is typically preferred if patient positioning allows for it. In one study, 52% of patients monitored with facial nerve stimulation had residual paralysis compared to 22% in those who had ulnar nerve monitoring [3]. Thus, if the facial nerve is utilized, ulnar nerve stimulation should still be employed to confirm the reversal of the neuromuscular blockade.
The gold standard for assessing neuromuscular blockade involves Train-of-Four monitoring. This technique evaluates the response of peripheral nerves to electrical stimulation, measuring the ratio of muscle twitches in response to four successive stimuli. Monitoring the decreasing amplitude in muscle response helps anesthesiologists gauge the level of neuromuscular blockade and tailor the administration of blocking agents or reversal agents accordingly [4]. EMG monitors placed over the ulnar nerve can record the same train of four count and ratio. As aforementioned, relying solely on clinical signs, such as observed movement or respiratory effort, can be misleading. Objective monitoring provides a more accurate assessment of neuromuscular function, allowing providers to titrate muscle relaxants precisely.
Different neuromuscular blocking agents (NMBAs) have varying durations of action and moreover muscle groups respond differently to NMBAs. After administration, the neuromuscular block typically occurs fastest in central muscles including the larynx and diaphragm, and later in the peripheral muscles. However, the central muscles, like the diaphragm, recover faster as they are more resistant to effects of NMBAs [5]. This is important for successful intubation and safe extubation. If a train-of-four ratio is above 0.9, it can be assumed the diaphragm has recovered from the neuromuscular blockade. Lastly, the use of reversal agents, such as neostigmine and sugammadex, is common to rapidly counteract the effects of NMBAs at the end of surgery [6]. Monitoring the response to these reversal agents ensures effective reversal, prevents residual blockade, and ensures safe extubation.
References
- Fuchs-Buder T, Romero CS, Lewald H, Lamperti M, Afshari A, Hristovska AM, Schmartz D, Hinkelbein J, Longrois D, Popp M, de Boer HD, Sorbello M, Jankovic R, Kranke P. Peri-operative management of neuromuscular blockade: A guideline from the European Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol. 2023 Feb 1;40(2):82-94.
- Hayes AH, Mirakhur RK, Breslin DS, Reid JE, McCourt KC. Postoperative residual block after intermediate-acting neuromuscular blocking drugs. Anaesthesia. 2001 Apr;56(4):312-8.
- Thilen SR, Hansen BE, Ramaiah R, Kent CD, Treggiari MM, Bhananker SM. Intraoperative neuromuscular monitoring site and residual paralysis. Anesthesiology. 2012 Nov;117(5):964-72.
- Lee CM. Train-of-4 quantitation of competitive neuromuscular block. Anesth Analg. 1975 Sep-Oct;54(5):649-53.
- Wright PM, Caldwell JE, Miller RD. Onset and duration of rocuronium and succinylcholine at the adductor pollicis and laryngeal adductor muscles in anesthetized humans. Anesthesiology. 1994 Nov;81(5):1110-5.
- Hunter JM. Reversal of neuromuscular block. BJA Educ. 2020 Aug;20(8):259-265. doi: 10.1016/j.bjae.2020.03.008. Epub 2020 Jul 1.
- Renew JR. Monitoring neuromuscular blockade. In: UpToDate, Connor RF (Ed), Wolters Kluwer. (Accessed on Jan 26, 2024.)






Recent Comments